
State Health Coverage Reporting Requirements
February 16, 2024
Pharmacy Costs Under Scrutiny in Recent Litigation
February 27, 2024On January 22, 2024, the Departments of Labor, Health and Human Services, and the Treasury (collectively, “the
Departments”) answered a new round of FAQs, providing additional guidance on the Affordable Care Act (“ACA”)’s requirement for non-grandfathered medical plans to cover certain preventive services including contraceptives, without cost-sharing. These FAQs answer questions from stakeholders to help people understand the contraceptive coverage mandate and promote compliance by providing an alternate method of compliance. It should be noted that religious employers, certain non-profit religious organizations, and closely held for-profit entities can exclude contraception.
Background
Plans and issuers must cover at least one form of contraception in each of the following categories:
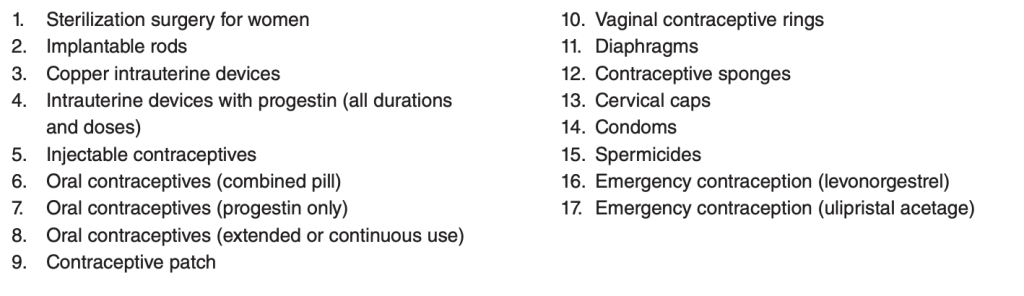
Plans must also cover any additional contraceptives approved, cleared, or granted by the FDA (including newer contraceptive products) so long as the individual’s attending provider determines such care as medically appropriate and necessary. Plans may apply reasonable medical management techniques for newer products and procedures only if there exists at least one other substantially similar product or service available and medically appropriate, and that similar product or service is covered





