
Supreme Court Effectively Ends OSHA Vaccination Emergency Temporary Standard
January 24, 2022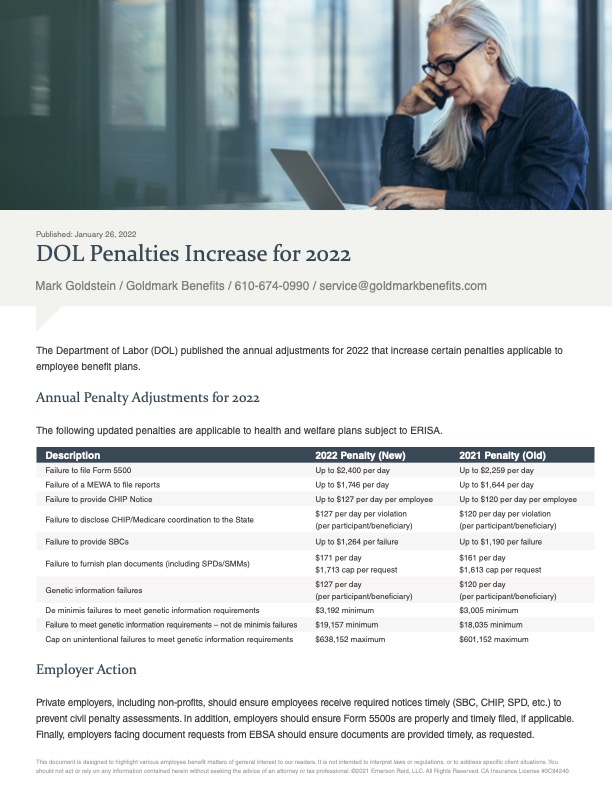
DOL Penalties Increase for 2022
February 1, 2022On January 14, 2022, the Secretary of Health and Human Services (“HHS”) renewed the COVID-19 pandemic Public
Health Emergency, effective January 16, 2022. This will once again extend the Public Health Emergency period for
an additional 90 days and as a result, numerous temporary benefit plan changes will remain in effect.
Important Definitions
Emergency Period: HHS issued a Public Health Emergency beginning January 27, 2020. This Emergency Period is now set to expire April 16, 2022 (unless further extended or shortened by HHS).
Outbreak Period: The Outbreak Period started March 1, 2020.The end date is applied on a participant-byparticipant basis and is the earlier of 1) one year after the date the participant was eligible for relief, and 2) 60 days after the announced end of the National Emergency.
While there are other temporary benefit plan provisions and changes that are allowed due to the Public Health
Emergency, summarized below are only those provisions directly impacted by the Emergency Period extension.
Benefit Plan Changes in Effect Through the End of the Emergency Period
• COVID-19 Testing. All group health plans must cover COVID-19 tests and other services resulting in the order for a test without cost-sharing (both in-network and out-of-network), prior authorization, or medical management and includes both traditional and nontraditional care settings in which a COVID-19 test is ordered or administered.
• Over-The-Counter (“OTC”) COVID-19 Testing: Beginning January 15, 2022 all group health plans must cover OTC COVID-19 tests for diagnostic purposes without cost-sharing (both in network and out-of-network), prior authorization, medical management and without requiring medical assessment or prescription. Plans may limit the reimbursement for the purchase of OTC COVID-19 tests to eight tests per month per enrollee. Plans with established networks and direct coverage may limit the reimbursement for out-of-network OTC COVID-19 tests to up to $12 or the actual cost of the test, if less.
• COVID-19 Vaccines. All non-grandfathered group health plans must cover COVID-19 vaccines (including cost of administering) and related office visit costs without cost-sharing; this applies, to both in-network and out-of-network providers, but a plan can implement cost-sharing after the Emergency Period expires for services provided out-of-network.
• Excepted Benefits and COVID-19 Testing. An Employee Assistance Program (“EAP”) will not be considered to provide significant medical benefits solely because it offers benefits for diagnosis and testing for COVID-19 during the Emergency Period and therefore, will be able to maintain status as an excepted benefit.
• Expanded Telehealth and Remote Care Services. Large employers (51 or more employees) with planyears that begin before the end of the Emergency Period may offer telehealth or other remote care services to employees (and their dependents) who are not eligible for other group health plan coverage offered by the employer.
• Summary of Benefits and Coverage (“SBC”) Changes. Group health plans may notify plan members of changes as soon as practicable and are not held to the 60-day advance notice requirement for changes affecting the SBC during the plan year or for the reversal of COVID-19 changes once the Emergency Period expires, provided the plan members are timely made aware of any increase and/or decrease in plan benefits summarized on the SBC.
• Grandfathered plans. If a grandfathered plan enhanced benefits related to COVID-19 for the duration
of the Emergency Period (e.g., added telehealth or reduced or eliminated cost-sharing), the plan will not
lose grandfathered status if the changes are later reversed when the Emergency Period expires.
Benefit Plan Changes in Effect Through the End of the Outbreak Period
On an individual basis, group health plans, disability, and other employee welfare benefit plans will disregard
the period of one year from the date an individual is first eligible for relief, or 60 days after the announced end of
the National Emergency, whichever occurs first, when determining the following:
• COBRA. Timeframe for the employer to provide a COBRA election notice; the 60-day election period
for a qualified beneficiary to elect COBRA; the COBRA premium payment deadlines (45 days for initial payment, 30-day grace period for ongoing payments); the deadline to notify the plan of qualifying events or disability determinations.
• HIPAA Special Enrollment. 30 days (60 days for Medicaid/CHIP events) to request a special enrollment right due to loss of health coverage, marriage, birth adoption, or placement for adoption.
• ERISA Claims Deadlines. Timeframes to submit a claim and to appeal an adverse benefit determination. For non grandfathered medical plans, timeframes to request external review and perfect an incomplete request.
• This includes claim deadlines for a health FSA or HRA that occur during the Outbreak Period.
Fiduciary Relief of Certain Notification and
Disclosure Deadlines for ERISA Plans.
A plan will not be in violation of ERISA for a failure to timely furnish a notice, disclosure, or document throughout the duration of the Outbreak Period if the plan and fiduciary operate in good faith and furnish the notice, disclosure, or document as soon as administratively practicable (which may include the use of electronic means such as email and text messages).
Employer Action
Employers should continue to adhere to the national pandemic-related benefit changes and expanded timeframe for providing COVID-19 testing and vaccinations and other required plan notifications. State and local emergency measures may expire at different times and could impact employee benefit plans (such as insured group health plans) and other state and/or local programs (such as paid leave) differently than the timeframes required under federally regulated program requirements.





